FAQs
Frequently Asked Questions
- Men we interviewed as part of our research
- Local Advisory Group members during our monthly meetings
- Other questions that have come up over the course of our involvement in this work
Questions About Screening Eligibility
You won’t be asked directly about your sexual orientation during screening. The questions all donors are asked, regardless of gender or sexuality, on the screening questionnaire that you fill out on a tablet, or at home are:
→In the last 3 months, have you had a new sexual partner?
If yes, then: In the last 3 months did you have anal sex?
→In the last 3 months, have you had more than one sexual partner?
If ‘yes, then: In the last 3 months did you have anal sex?
Check out the Am I Eligible to Donate Plasma or Blood page on our site. You can also browse the other sections of our site for a deeper dive into questions about eligibility. Check out the pages under the Am I Eligible to Donate section for more information.
All infections have what is known as a “window period” – the time between the start of the infection and the point where tests can reliably detect it. During that window, the infection might not be detected by tests even though it is present in the blood. Screening questions, including the new ones about anal sex with new or multiple partners in the last 3 months, are mostly to reduce the risk of window period infections.
Canadian Blood Services has established 3 months as the minimum window period for Hepatitis B and Syphilis (HIV and Hepatitis C are actually shorter). The 3-month waiting period was chosen as an interim step between the previous 12-month period and the upcoming sexual behaviour-based screening criteria (source). Mathematical modelling showed that the change from 12 months to 3 months would not significantly increase risk, and that change was approved by Health Canada. The new screening questions ask specifically about anal sex with new or multiple partners in the past three months because anal sex is shown in the research to be associated with the highest risk of HIV infection.
Very generally speaking, anal sex has a high risk for HIV infection. This article from the Centre for Disease Control explains a few very basic things about HIV risk in simple terms.
This is a bit complicated. Unless the screening asks about a specific type of sex (e.g., anal sex), sexual contact includes oral, anal and vaginal sex.
There is a suggestion that oral sex may post a slight risk for HIV transmission, although researchers have found it difficult to quantify exactly what that risk is compared to vaginal and anal intercourse (check out this report for more info). It is difficult to study whether HIV can be passed on during oral sex because many people have oral sex as well as other kinds of sex in the same encounter (Source: PHAC, 2012). Anal sex is shown in the research to be associated with the highest risk of HIV infection.
For the new sexual behavior based screening, donors with new partners or multiple partners in the last three months, will be asked an additional question about anal sex. Donors who answer yes to this question will be ineligible to donate for three months. For donors who have not had a new sexual partner or multiple partners in the last three months the question about anal sex will not be asked.
Canadian Blood Services is an independent, non-profit organization, regulated by Health Canada. It was created to be at arm’s length from the government because of what happened in the past. However, because Health Canada oversees anything to do with the health of Canadians, Canadian Blood Services is required to get their approval on any changes they make. In order to make changes to criteria, Canadian Blood Services must prove – with donation-specific data – that the change will not decrease blood safety.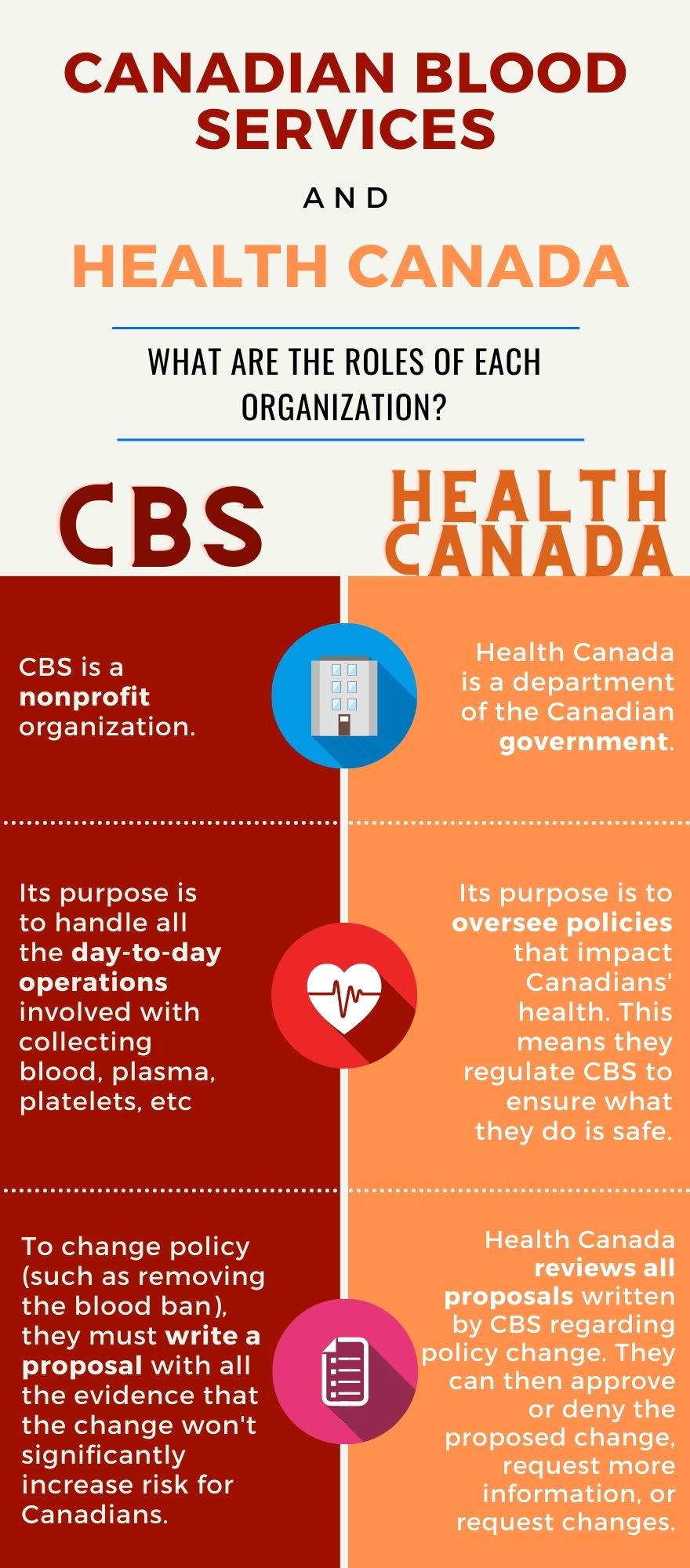
The official answer is this: there is research that shows that all donors, not just men, have an increased risk of sexually transmitted infections when they have multiple partners.
However, since the sexual behaviour based rules came into effect on September 11th, 2022, this question has gotten a bit trickier to answer. Depending on the individual situation, how frequently, and what kinds of sex a throuple/poly person is having, they may still be eligible to donate. The bottom line is that you can’t have had anal sex with new or multiple partners in the past 3 months. All that said, people in these kinds of relationships may well find themselves unable to donate, which is bull. If three people in a relationship are only having sex with each other, it stands to reason that risk would be the same as it would for two people who are only having sex with each other. Sadly, we’re chalking this up to heteronormative monogamy standards and expectations of relationships – another rule that needs to change!
Questions About Covid-19 and Donation
Things are constantly changing with Covid-19. Rules around giving blood or plasma have changed over the course of the pandemic – and we expect that this will continue to be the case. Instead of updating our site with the latest rules related to Covid, below we will direct you to various parts of Canadian Blood Services’ website for the most up-to-date information.
Most information about Covid-19 and donation can be found here. This includes information about safety protocols within the donor centre, waiting periods after being sick with Covid, and much more.
For information about Covid-19 and vaccines, please see here.
For a list of questions and answers with regards to organ and tissue donation, please see here.
Canadian Blood Services is part of a study to see whether plasma given by someone recovered from Covid-19 can be used to treat someone who is sick with Covid-19. For more information on the research, check out here.
General Questions About Canadian Criteria for Men Who Have Sex with Men
Since the ‘tainted blood tragedy’ in the 1980s, Canada’s blood system has been extremely risk-averse. The fear of repeating the tragedy of the 80s has led to a very conservative approach to changes. Gay, bi, and men who have sex with men have borne the burden, despite much of the devastation of the tainted blood tragedy being due to failures within the blood system at that time (like not implementing testing as soon as it became available).
Fear and extreme caution led to an incremental approach to changing the criteria. Men who had had sex with a man even once since 1977 were originally permanently banned from donating. This was gradually reduced to a 5 year, 1 year, then 3 month waiting period between anal or oral sex with another man and being allowed to donate. Each time the waiting period was shortened, Canadian Blood Services had to provide Health Canada with data to show that each change did not increase risk of infections in the blood supply. This in turn increased confidence in the new blood system and in the safety of changes to these criteria. Canadian Blood Services was also required to gain the support of both patient and community groups for each change.
Other countries also followed an incremental approach, sometimes in fewer steps. Canadian Blood Services is part of an international alliance of blood operators that share information and research. Canadian Blood Services’ policies have progressively changed more or less in line with other G7 countries. For more details about other countries’ policies on blood donation for gbMSM, check here.
The latest change to sexual behaviour based screening questions was enabled by new data from both the Canadian research studies and the research studies that supported a similar change in policy in the UK. You can read more about these changes on Canadian Blood Services’ website: An update on our journey to build a more inclusive blood system.
Questions About Safer Sex Practices
Why don’t the screening criteria ask about specific sexual health behaviours, like using condoms, regular testing, using PrEP or following U=U? We understand that is seems a bit backward that the recommended safer sex practices for gbMSM are not the primary behaviours that are used in donor screening. Below we have more info in some of these specific areas.
We understand it seems a bit backwards that the recommended safe sex practices for gbMSM are not the primary behaviours that are used in donor screening. Check out the sections below for more information on these topics.
Canadian Blood Services doesn’t ask about condom use because condoms are not completely reliable. Condoms can slip, break, or leak, making them ineffective. Some of the people interviewed for this research project wanted screening for plasma donation to look more like STI screening. This would be more like an interview, with questions like “Tell me about your sex practices: do you always use a condom? Does it ever break? How often do you take recreational drugs with sex?” This kind of interview can give a more detailed, nuanced and individual risk assessment. However, it would require a lot of questions, and Canada would have to better resourced (give more money to) the blood systems to provide this kind of individual risk assessment as each screening would take more time.
The information that public health has about your sexual health status is confidential. Due to privacy laws, they cannot release it without your consent. That’s why, under the current regulations of the blood system, Canadian Blood Services has to use their own tests – they can’t use test results from any other organizations or agencies.
There are several options:
- As of November 2020, the INSTI HIV self-test has been approved for use in Canada. You can purchase it directly from the manufacturer.
- You can ask your family doctor.
- Some people may prefer an anonymous method. Anonymous tests can be done at various health clinics (see below).
In London: London InterCommunity Health Centre (LIHC) is a great resource, with 10 different sites across the city.
In Calgary: HIV Community Link (HIVCL) provides a list of locations that perform testing, updated with COVID-19 restrictions.
Questions About Donating Blood/Plasma
Please see here for more info.
Please see here for more info.
Because of the COVID-19 pandemic, there are restrictions on the number of people that can be in the donor centre to allow for social distancing. If you and your friend both make an appointment to donate together at the same time, the staff will try their best to seat you together.
Based on our interviews and talks with guys in the GBT2Q+ communities, some suggestions for making donating more safe, comfortable, and fun include:
- going with a friend
- making donating a social outing with a friend group (for example, your study group, volleyball team, co-workers, or book club)
- pairing donating with something fun like a mixer at a sex toy shop
Check out our full list of suggestions from folks in the communities!
See the sections about what plasma is and how it helps for more information.
All blood types are equally needed for source plasma donations made at plasma donor centres.
No. Canadian Blood Services’ policy is not to pay people for plasma (or blood). They rely on volunteers to donate plasma and blood. You can read more about Canadian Blood Services’ views on paid plasma donation here.
Each province decides whether people can be paid for plasma donation. Currently Ontario does not allow people to be paid for their plasma. However, Alberta recently allowed plasma donors to be paid (see here for more details). An independent company is setting up locations in Calgary and Edmonton, which will pay people for their plasma. At the time of writing, this company uses a very outdated screening criterion. They do not allow any man who has had sex with another man even once since 1977 to donate. They do not mention evolving this criterion anywhere on their website.
No, your donation would not be used for cosmetic purposes– only for health care. If you want to know more about this technique, look here. Plasma collected by Canadian Blood Services is sent to fractionators. The fractionators process it to create different plasma protein products, like immunoglobulin. Those products are then returned to Canadian Blood Services to manage and distribute.
