Organs Tissues Stem Cells
Organs, Tissues & Stem Cells
Our research team spoke with Organ Donor Specialist Physician, Dr. Murdoch Leeies and with hematologist, Dr. Warren Fingrut, about the practicalities of organ, tissue and stem cell donations. Dr. Murdoch is doing research to improve organ donation policies and Dr. Fingrut is the director of Stem Cell Club, a donor recruitment organization that advocates for a more inclusive blood system in Canada.
Official Policy:
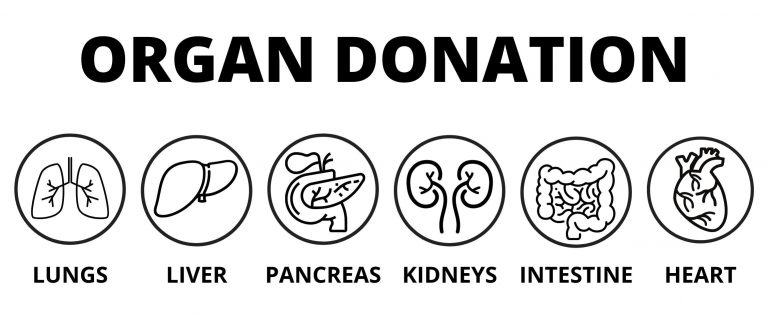
For organs, tissues, and stem cells, sexually active gbMSM can register to be a donor, as long as you meet other requirements (for example, stem cell donors must be between the ages of 17 and 35). However, tissue donated by sexually active gbMSM is not used (see the section on tissues below for more info).
A specific patient and donor match is needed for organ, tissue, and stem cell donation. These matches are hard to find, so these donations are handled differently from blood and plasma. Each donor is individually risk-assessed…which begs the question: why aren’t ALL donors individually risk-assessed, even for blood and plasma? If the blood system was funded for individual risk assessment, we wouldn’t end up with blanket exclusions of entire groups of people! Donors are assessed individually by the doctor doing the transplantation, in discussion with the patient who will be receiving the transplant. This is one reason why screening policies are different for gbMSM who wish to donate plasma versus organ, tissue, and stem cells donations.
If the doctor decides that the donor is a good match, they have a conversation with the recipient to advise them on the match. The doctor would tell the recipient about any characteristics of the donor that do not meet the usual Canadian Standards Association criteria. This includes telling the recipient if the donor identifies as gbMSM. The patient would need to accept this additional “risk”. The “increased risk” categorization of gbMSM for organ, tissue, and stem cell donation is stigmatizing and in need of change. Risk should be evaluated on an individual basis, regardless of sexual orientation, as there are many factors to consider. For example, a straight person who has multiple new partners would be at higher risk of an STI than a gay man who has been in an exclusive relationship for years.
Drs. Leeies and Fingrut explained that it required extra paperwork, but that there were no practical barriers for gbMSM to donate.
What about in the case of organ donation?
Potential recipients would be told that they were being offered an organ from an “increased risk donor”. This can lead to the donor being outed. This is a risk in both living donation (meaning the donor is still alive, such as for some kidney or liver transplants) and paired deceased donation (which is when the donor has died). In living donation, the donor usually knows the potential recipient.
For a good article on the details of organ donation by gbMSM, see this one in Xtra. Content Warning: The information in the Xtra article can be extremely upsetting. If you experience any distress, we have a list of mental health resources you may find useful here.
What about in the case of stem cells?
Anyone between the ages of 17-35, who is not living with HIV or a few other conditions, can register to donate stem cells. It can take years for a match to be found – if one is found at all. A physician then completes a full health assessment to determine whether the registered person can be a donor. The doctor would counsel the recipient that this donor is their best chance. The donor and recipient are then both prepped for donation. As part of preparation, the donor would be asked to avoid “high risk activities” in the weeks leading up to the donation that could impact on the safety of the recipient (including but not limited to unprotected sex with a new partner). There is no specific policy for the counselling of gbMSM donors – it is up to the discretion of the transplant physician based on their assessment. Check out Saving Lives With Pride to read more about gbMSM stem cell donation.
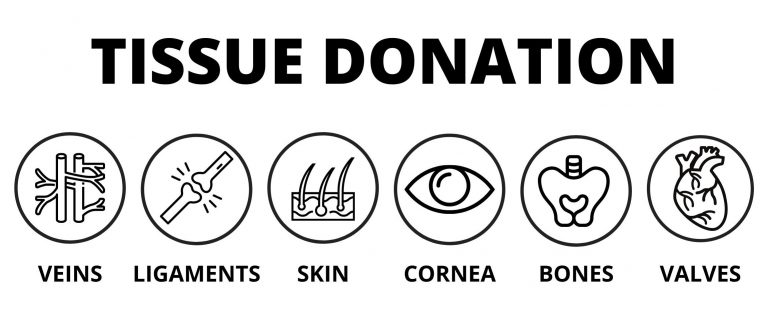
What about in the case of tissue donation?
While it is legal for gbMSM to donate tissue, tissue programs will not accept tissue from gbMSM donors (tissues are things like cornea, heart valves, skin, bone, and tendons). This includes tissues donated by gbMSM who have had sex with another man in the last 5 years. Tissue is needed less urgently than organs and this is the rationale for why more progressive policy regarding gbMSM tissue donor has been stalled. Specifically, the (shocking) rationale is that the “risk” of using transplanted tissue from sexually active gbMSM outweighs the benefit. However, the risk is not backed-up by data. Not allowing men to donate tissues if they’ve had sex with another man within 5 years is not evidence-based and it stigmatizes sexually active gbMSM.
Overall, an equitable, evidence-based screening policy for donors regardless of sexual orientation or gender is ugently needed for stem cell, tissue, and organ donation.
